Article Plan: Quadriceps Tendonitis Exercises PDF
This article details a structured rehabilitation approach, outlining exercises for a downloadable PDF guide, focusing on phases post-injury or surgery․
Quadriceps tendonitis, an overuse injury, causes pain just above the kneecap where the quadriceps tendon attaches․ This condition impacts individuals engaging in frequent jumping, running, or explosive movements․ Effective rehabilitation, often guided by a PDF exercise plan, is crucial for recovery․
Understanding the progressive nature of this injury is key; a phased approach—spanning from initial range of motion exercises to advanced strengthening and functional training—is generally recommended․ Protocols like the Alfredson protocol, emphasizing eccentric strengthening, are frequently incorporated․
A well-designed PDF provides a convenient, accessible resource for patients to follow their rehabilitation program consistently․ It’s vital to avoid aggravating exercises like deep squats and lunges during the healing process, prioritizing proper form and technique throughout each phase․ This article will explore a comprehensive rehabilitation pathway, suitable for creating a personalized PDF guide․
Understanding the Quadriceps Tendon
The quadriceps tendon is a strong fibrous cord connecting the quadriceps muscles (front of the thigh) to the patella (kneecap)․ Its primary function is to extend the knee, enabling activities like walking, running, and jumping․ This tendon withstands significant force, making it susceptible to inflammation and degeneration – leading to quadriceps tendonitis․
A PDF exercise guide must acknowledge the tendon’s role in knee stability and movement․ Damage occurs through repetitive strain, causing microscopic tears․ Understanding its anatomy is crucial for targeted rehabilitation․
Rehabilitation protocols, often detailed in a PDF, aim to restore the tendon’s strength and flexibility․ Eccentric exercises, a cornerstone of recovery, specifically target the tendon’s ability to withstand load․ A comprehensive PDF will illustrate proper technique to maximize effectiveness and minimize further injury risk, guiding users through a safe and progressive recovery․
Causes and Risk Factors of Quadriceps Tendonitis
Quadriceps tendonitis typically arises from overuse, repetitive strain, or sudden increases in activity levels․ Sports involving frequent jumping – like basketball or volleyball – significantly elevate risk․ Insufficient warm-up routines and inadequate stretching contribute to tendon stress;

A PDF exercise guide should highlight these contributing factors․ Other risks include muscle imbalances, improper biomechanics, and pre-existing conditions like arthritis․ Age-related tendon degeneration also plays a role, reducing tissue elasticity․
Post-operative rehabilitation, detailed in a PDF protocol, must consider individual risk factors․ A thorough assessment is vital before initiating exercises․ The PDF should emphasize gradual progression, avoiding activities that exacerbate pain․ Understanding these causes informs a personalized exercise plan, optimizing recovery and preventing recurrence․

Symptoms of Quadriceps Tendonitis
Quadriceps tendonitis manifests primarily as pain just above the kneecap, often worsening with activity․ Initially, discomfort may only occur during or after exercise, but it can progress to constant pain even at rest․ A PDF exercise guide should clearly explain these symptom patterns․
Individuals may experience tenderness to the touch over the quadriceps tendon․ Stiffness in the knee, particularly in the morning or after periods of inactivity, is common․ Swelling around the kneecap can also occur, though it’s usually mild․
A comprehensive PDF should detail how symptoms impact daily function․ Pain during activities like walking, running, or climbing stairs is typical․ Ignoring these signals can lead to chronic tendon issues․ Early recognition, aided by a PDF’s symptom checklist, is crucial for effective rehabilitation․

Diagnosis of Quadriceps Tendonitis
Diagnosing quadriceps tendonitis typically begins with a thorough physical examination by a healthcare professional․ This involves assessing pain location, range of motion, and tenderness along the quadriceps tendon․ A PDF exercise guide should emphasize the importance of professional evaluation․
Imaging tests, while not always necessary, can help confirm the diagnosis and rule out other conditions․ X-rays can exclude bone abnormalities, and MRI scans provide detailed views of the tendon, revealing inflammation or tears․
A PDF resource should highlight that accurate diagnosis is vital before starting any exercise program․ Self-diagnosis can be misleading․ Clinicians will assess gait and knee mechanics․ A detailed PDF can prepare patients for what to expect during the diagnostic process, ensuring informed participation in their rehabilitation․
The Role of a PDF Exercise Guide
A downloadable PDF exercise guide for quadriceps tendonitis serves as a crucial tool for patient education and adherence to a rehabilitation program․ It provides a structured, accessible resource outlining appropriate exercises, progression criteria, and important safety considerations․ The guide empowers individuals to actively participate in their recovery․
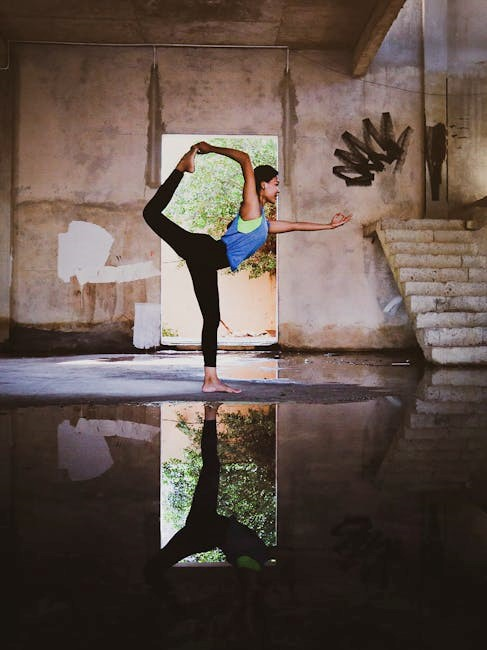
A well-designed PDF should include clear illustrations or videos demonstrating proper form for each exercise, minimizing the risk of re-injury․ It allows for convenient access to information outside of clinic visits, reinforcing learned techniques․
Furthermore, a PDF can be personalized by a physical therapist to address individual needs and goals․ It facilitates consistent exercise routines and tracks progress, ultimately optimizing outcomes․ The guide complements professional guidance, fostering a collaborative approach to healing․

Phase 1 Rehabilitation (0-2 Weeks Post-Injury/Surgery)
Initial rehabilitation (0-2 weeks) focuses on minimizing pain and inflammation while protecting the repaired tendon․ Weight-bearing is typically limited, as tolerated, utilizing crutches and a brace locked in full extension․ The goal is to gradually progress weight-bearing as pain allows․
Range of motion (ROM) exercises are initiated gently, focusing on achieving full knee extension and gradually increasing flexion․ Early strengthening involves isometric quadriceps contractions – tightening the muscle without moving the joint – and gentle ankle pumps to promote circulation․
Avoidance of exercises that overload the quadriceps and patellar tendons, such as squats and lunges, is critical during this phase․ The emphasis is on controlled movements and respecting pain boundaries, establishing a foundation for subsequent phases․

Weight Bearing and Bracing in Phase 1

Weight-bearing protocols during the initial 0-2 week phase are carefully managed, typically as tolerated with the assistance of crutches․ Full weight-bearing is generally not permitted immediately post-surgery or injury, prioritizing tendon protection․
A brace is crucial, initially locked in full extension to immobilize the knee and prevent stress on the healing tendon․ Gradual progression of weight-bearing is dictated by pain levels and the rehabilitation provider’s assessment of tissue healing․
The ability to discontinue crutches is determined by leg control and progress, guided by both the patient and physician․ Consistent use of the brace, locked in extension, is maintained throughout this initial phase, ensuring optimal tendon support and minimizing the risk of re-injury․
Range of Motion Exercises (Phase 1)
Early range of motion (ROM) exercises in Phase 1 focus on restoring basic knee movement without stressing the quadriceps tendon․ Gentle heel slides are initiated, progressing the knee bend as tolerated, always within a pain-free range․
Patellar mobilization is also key, carefully moving the kneecap in all directions to prevent stiffness and maintain joint mobility․ These movements should be performed slowly and gently, avoiding any forceful manipulation․
The goal is to achieve a comfortable, limited range of motion, prioritizing pain management and protecting the healing tendon․ Active quadriceps sets, without attempting to straighten the knee fully, help maintain muscle activation without excessive strain․ Consistent, controlled movements are vital during this initial stage․
Initial Strengthening Exercises (Phase 1)
Phase 1 strengthening focuses on isometric exercises, engaging the quadriceps without joint movement, minimizing stress on the healing tendon․ Quadriceps sets – tightening the thigh muscles while keeping the leg straight – are performed frequently throughout the day․

Gluteal squeezes and hamstring sets are incorporated to maintain overall leg muscle activation and stability․ Ankle pumps help improve circulation and reduce swelling․ These exercises are performed within a pain-free range, prioritizing muscle activation over significant resistance․
Avoid exercises like straight leg raises initially, as they can overload the quadriceps tendon․ The emphasis is on gentle muscle engagement to prevent atrophy and prepare for more advanced strengthening in subsequent phases․ Controlled, low-intensity contractions are crucial for safe and effective rehabilitation․
Phase 2 Rehabilitation (2-6 Weeks Post-Injury/Surgery)
Phase 2 marks a progression in weight-bearing and exercise intensity, building upon the foundation established in Phase 1․ Gradual increases in weight-bearing are implemented, guided by pain levels and functional progress, potentially transitioning from crutches to partial weight-bearing․
Range of motion exercises are advanced, incorporating gentle stretching to improve knee flexion and extension․ Strengthening exercises begin to include closed-chain activities, like mini-squats and leg presses with light resistance, carefully avoiding overload․
Focus remains on quadriceps strengthening, but with controlled movements and attention to proper form․ The goal is to restore functional strength and prepare the leg for more demanding activities in Phase 3․ Continued monitoring for pain and swelling is essential throughout this phase․
Progression of Weight Bearing (Phase 2)
Weight-bearing progression in Phase 2 is carefully managed, transitioning from the initial protected weight-bearing of Phase 1․ The aim is to gradually increase the load on the affected leg, guided by pain tolerance and functional improvements․
Initially, partial weight-bearing with crutches continues, with the goal of weaning off crutches as quadriceps control and pain allow․ The brace may remain locked in extension during early stages, providing stability․
Progression is individualized, based on the patient’s response to exercises and daily activities․ Clinicians monitor gait pattern and assess for any signs of increased pain or swelling․ Full weight-bearing is only permitted when adequate quadriceps strength and control are demonstrated, ensuring safe and effective rehabilitation․
Advanced Range of Motion Exercises (Phase 2)
Phase 2 introduces more challenging range of motion (ROM) exercises, building upon the foundation established in Phase 1․ The focus shifts towards restoring full knee flexion and extension, while minimizing stress on the quadriceps and patellar tendons․
Heel slides are progressed, increasing the range of flexion․ Gentle stationary cycling without resistance is introduced to promote smooth joint movement․ Wall slides are performed cautiously, ensuring proper form and avoiding pain․
Active-assisted ROM exercises, utilizing a towel or strap, can help improve flexion․ It’s crucial to avoid forceful stretching or movements that provoke pain․ The goal is to achieve a functional ROM necessary for daily activities, preparing the knee for more advanced strengthening exercises․
Strengthening Exercises – Focus on Quadriceps (Phase 2)
Phase 2 emphasizes progressive quadriceps strengthening, carefully avoiding exercises that overload the tendon․ Initial strengthening focuses on isometric exercises, such as quad sets – tightening the thigh muscles without moving the knee․ These are held for several seconds and repeated․
Short-arc quads, performed with a small range of motion, begin to build dynamic strength․ Straight leg raises, performed in various positions (supine, side-lying), further engage the quadriceps․
Resistance bands are introduced for gentle strengthening, focusing on extension and abduction․ Crucially, squats and lunges are avoided during this phase due to their high impact on the quadriceps and patellar tendons․ The aim is to gradually increase strength while protecting the healing tendon․
Phase 3 Rehabilitation (6-12 Weeks Post-Injury/Surgery)
Phase 3 focuses on restoring full function and preparing for return to activity․ Functional exercises are key, gradually reintroducing movements required for daily life and sport․ This includes controlled squats (initially shallow), step-ups, and controlled lunges – always monitoring for pain․
Proprioceptive training is vital to regain balance and coordination․ Exercises like single-leg stance, wobble board activities, and agility drills challenge the body’s awareness of joint position․
Progressive loading continues, increasing resistance and complexity of exercises․ The goal is to build strength, endurance, and confidence․ A gradual return to sport-specific activities is implemented, guided by pain levels and functional assessments․
Functional Exercises (Phase 3)
Functional exercises bridge the gap between controlled rehabilitation and real-world activities․ Begin with controlled squats, progressing in depth as tolerated, ensuring proper form to avoid overloading the quadriceps and patellar tendons․ Step-ups onto a low platform challenge strength and stability․
Controlled lunges, both forward and lateral, improve functional movement patterns․ Emphasis should be on maintaining alignment and avoiding pain․ Introduce agility drills like cone drills and shuttle runs to enhance coordination and responsiveness․
Simulate sport-specific movements gradually, if applicable․ This could involve light jogging, jumping, or cutting maneuvers, always monitoring for any discomfort․ The focus remains on quality of movement over quantity․
Proprioceptive Training (Phase 3)
Proprioception, or body awareness, is crucial for preventing re-injury․ Single-leg stance exercises, initially on a stable surface, challenge balance and stability․ Progress to unstable surfaces like a foam pad or wobble board to increase the difficulty․
Balance exercises can include reaching in different directions while maintaining single-leg stance․ Incorporate dynamic movements, such as tossing a ball while balancing, to further challenge proprioceptive abilities․
Plyometric exercises, like controlled jumps and hops, improve reactive strength and neuromuscular control․ Begin with low-impact plyometrics and gradually increase the intensity․ These exercises should only be introduced when pain-free and with adequate strength and control․
The Alfredson Protocol for Quadriceps Tendonitis
The Alfredson protocol is a well-regarded treatment for quadriceps tendonitis, focusing on eccentric strengthening․ It involves performing squats against a wall, slowly lowering the body weight over several seconds, and then using both legs to return to the starting position․
The protocol consists of three phases: Phase 1 involves performing 15 repetitions with both legs, then one leg at a time․ Phase 2 adds weight by holding a weight or using a weighted vest․ Phase 3 increases the difficulty by performing the exercise on an incline․
It’s recommended to perform the exercises daily, and pain levels should be monitored․ The protocol is designed to gradually load the tendon, promoting healing and reducing pain․ Consistency is key for optimal results․
Eccentric Strengthening Exercises
Eccentric exercises are crucial for quadriceps tendonitis rehabilitation, focusing on lengthening the muscle while contracting․ A primary example is the decline squat, performed by slowly lowering into a squat position and using both legs to return to standing․
Another effective exercise is the eccentric step-up, where you step up onto a platform with one leg and slowly lower yourself down, controlling the descent․ These exercises target the quadriceps and patellar tendons, promoting collagen realignment and strengthening․
Start with a low number of repetitions and gradually increase as tolerated, prioritizing proper form over quantity․ Pain should be monitored; a slight discomfort is acceptable, but sharp pain indicates the need to reduce intensity; Consistent eccentric training is vital for long-term recovery․
Exercises to Avoid During Rehabilitation
During quadriceps tendonitis recovery, certain exercises can exacerbate the condition and hinder progress․ High-impact activities like jumping, running, and plyometrics should be avoided initially, as they place significant stress on the tendon․
Exercises that create overload on the quadriceps and patellar tendons, such as deep squats and lunges, are also contraindicated, especially in the early phases of rehabilitation․ These movements can increase pain and inflammation․
Avoid straight leg raises without proper control, as they can strain the tendon․ Focus on controlled movements and gradually progress the intensity as healing occurs․ Prioritize exercises that minimize stress on the affected area and promote gradual strengthening․
Importance of Proper Form and Technique
Maintaining correct form during exercises is paramount for effective rehabilitation and preventing re-injury․ Incorrect technique can place undue stress on the quadriceps tendon, hindering healing and potentially worsening symptoms․
Focus on controlled movements, avoiding jerky or rushed motions․ Engage core muscles to stabilize the body and ensure proper alignment throughout each exercise; Pay close attention to knee alignment, preventing valgus or varus stress․
Consider working with a physical therapist to learn proper form and receive personalized guidance․ They can assess your technique and provide feedback to optimize exercise effectiveness and minimize risk․ Prioritize quality over quantity, ensuring each repetition is performed correctly․
Creating a Personalized PDF Exercise Plan
A tailored PDF exercise plan is crucial for optimal recovery from quadriceps tendonitis, acknowledging individual needs and progress․ Begin with a thorough assessment of your current functional level, pain levels, and range of motion․
The PDF should clearly outline each exercise, including detailed instructions, images or videos demonstrating proper form, and specific sets and repetitions․ Categorize exercises by rehabilitation phase (Phase 1, 2, 3) for progressive overload․
Incorporate a tracking system within the PDF to monitor progress, noting pain levels, completed sets, and any modifications made․ Regularly review and adjust the plan based on your response to treatment, consulting with a physical therapist for guidance․
Resources for Downloadable PDF Guides
Finding reliable PDF guides for quadriceps tendonitis exercises requires careful selection․ Many healthcare providers create customized plans for their patients, offering a strong starting point․
Online resources, such as hospital websites and physical therapy clinics, often provide downloadable protocols․ Search for guides specifically outlining post-operative rehabilitation for patella/quad tendon repairs, ensuring they align with your situation․
Consider resources focusing on the Alfredson protocol, a well-regarded eccentric strengthening program․ Always prioritize guides created by qualified professionals and review them with your physical therapist before starting any new exercise regimen․
Remember that a generic PDF may need personalization to address your specific needs and progress;
Long-Term Management and Prevention
Sustained quadriceps tendon health necessitates ongoing commitment beyond initial rehabilitation․ Consistent eccentric strengthening, like the Alfredson protocol, helps maintain tendon resilience and prevent re-injury․
Prioritize proper warm-up and cool-down routines before and after physical activity․ Incorporate regular stretching to maintain flexibility in the quadriceps and surrounding muscles․
Gradual progression of activity levels is crucial; avoid sudden increases in intensity or duration․ Pay attention to your body and modify activities if pain arises․
Maintaining optimal weight reduces stress on the knee joint․ Consider supportive footwear and address any biomechanical imbalances through targeted exercises․
Proactive management ensures long-term function and minimizes the risk of chronic tendon issues․
